Pregnancy and the COVID Vaccine
Katie Harkess, MD
The past year has brought a lot of uncertainty to our lives. Given that pregnancy is already an uncertain time, the unknown surrounding COVID and the COVID vaccine can understandably lead to anxiety. Should you get this vaccine or not? Is the vaccine safe? With this blog, we hope to be able to shed some light on that question.
When patients walk into our office, the first question that they often have regarding the vaccine is, “How does this vaccine work?” The COVID vaccines are mRNA vaccines. Because these vaccines are the first mRNA vaccines on the market, there are a lot of questions regarding how they work. The vaccine contains a small amount of genetic material called mRNA. The best way to think about mRNA is as a recipe or as an instruction manual. Once you get the vaccine, the mRNA is taken up by your cells and acts as an instruction manual for your cells to make spike protein, a protein that is found on the COVID virus. Once your cells make the spike proteins, they present them to your immune cells, which then make antibodies against COVID. So, if you contract COVID, your body has the antibodies ready to go to fight the virus! After the mRNA has done its job, it is quickly degraded by your cells. Therefore, there is no evidence that it crosses the placenta. There are two important things to remember when considering these vaccines. First, because this vaccine does not contain a live COVID virus, it cannot give you COVID. In addition, because the mRNA is never taken into your cell’s nucleus, it does not have the ability to change your DNA. This new technology is very exciting because mRNA vaccines give us a much more efficient way to produce vaccines than previous vaccine technology using live or inactivated virus.
There have been two vaccines that have been approved for emergency use by the FDA. These vaccines have been produced by Pfizer and Moderna. The Pfizer vaccine is given in two doses 21 days apart and has been approved for use in people ages 16 and older. In the trials, the Pfizer vaccine was found to be 95% effective. To put that in perspective, consider that according to the CDC, the 2019-2020 flu vaccine was 39% effective. The Moderna Vaccine has been approved for people aged 18 and older. It is given in 2 doses 28 days apart and was found to be 94.5% effective in trials. Once you start a vaccine series, you should complete the series using the same manufacturer. Both doses in the series are necessary to receive full protection. If more than 21 or 28 days have passed since your first vaccination, the second dose should be given as soon as possible, but no doses need to be repeated.
The natural next question from our patients has been, “Is it safe?” Unfortunately, pregnant women were not included in the COVID vaccine trials. There are further ongoing studies, but the safety data is not yet available. However, the American College of Ob/Gyns, the American Society of Reproductive Medicine, and the Society for Maternal-Fetal Medicine all recommend that women who are trying to conceive, pregnant women and lactating women who are eligible for the vaccine should be offered the vaccine, even if they have previously had COVID. In addition, the current guidelines from these societies do not recommend waiting a specific amount of time to try to conceive after vaccination. But, what does that mean for you?
We know that pregnant women are at risk of having more severe disease if they contract COVID-19. Many reports have shown that pregnancy women are 3x more likely to need an ICU admission compared to non-pregnant women if they contract COVID. Depending on your health history and other underlying conditions, your risk of severe disease may be even higher. Thus, when deciding whether or not to receive the vaccine, we must consider four factors: 1) the level of activity of the virus in the community 2) the potential efficacy of the vaccine 3) the risk and potential severity of maternal disease, including the effects of disease on the fetus and newborn and 4) the safety of the vaccine for the pregnant patient and the fetus.
Unfortunately, the level of activity in our community is currently high, and we know that both vaccines have about a 95% efficacy rate. Thus, a lot of the decision is likely based on the potential risk of maternal disease and the safety of the vaccine for the pregnant patient. It is important to recognize that because the vaccine does not contain live virus, it is not thought to cause an increase in infertility, miscarriage, stillbirth or congenital abnormalities. Therefore, your individual factors as a patient will often dictate whether or not you receive the vaccine. What are your underlying health conditions that increase your risk of having severe disease? What is your risk of contracting the disease? We recognize that the risk of someone who works from home may be different than the risk of someone who works in healthcare.
If you decide to receive the vaccine during pregnancy, when is the best time to get it? At this time, there is not a recommendation for optimal timing of vaccine administration in pregnancy. However, the COVID vaccine should not be given within 14 days of another vaccine, which should be taken into consideration when giving other vaccines in pregnancy. Thus, the influenza and Tdap vaccine should not be given within 14 days of the COVID vaccine.
When taking all of these factors into consideration, we encourage you to talk to your provider at your next appointment about whether or not to receive the COVID vaccines and when to receive the vaccine. There is so much individualization that goes into this decision. We know that this is a personal decision, and we encourage you to ask questions and let us help guide you in your decision making. In the meantime, keep up the handwashing, maintain social distance and mask up! As always, we are here for you regarding any COVID or pregnancy-related questions!
Katie Harkess, MD
For more information regarding the COVID vaccine:
Dr. Neil Lamb of HudsonAlpha Institute for Biotechnology shares more information regarding COVID and the COVID vaccines in easy-to-understand videos:
https://hudsonalpha.org/beyond-the-blog/
Dr. Natalie Crawford, a board certified Ob/Gyn and reproductive endocrinologist and infertility specialist based out of Austin, TX, shares more information regarding COVID, the COVID vaccine and reproductive health on her YouTube channel:
https://www.youtube.com/channel/UCRZamIB-DWuVPJuc0bKhwzg/videos
A decision making guide for pregnant women about receiving the vaccine from the University of Massachusetts Medical School – Baystate:
https://www.baystatehealth.org/-/media/files/covid19/vaccine-info-for-pregnant-people-updated-12-28.pdf?la=en
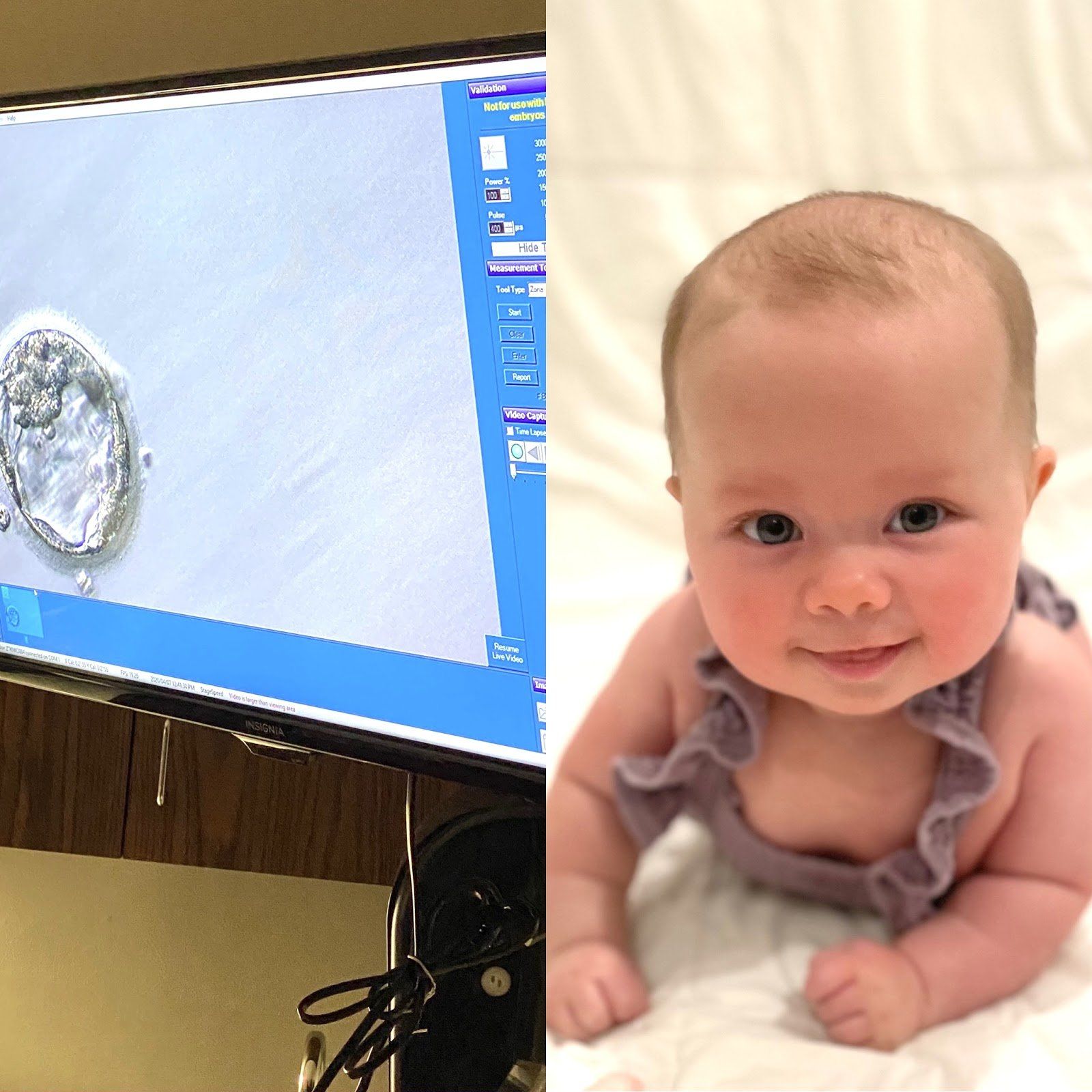
It is " Infertility Awareness Week ." Does it surprise you to know that 1 in 8 couples are inflicted by some sort of infertility? You will notice throughout my story, I may use words different than what you are used to hearing. I will not say 1 in 8 "struggle", because that implies that if we fought just a little harder, struggled against it a little longer, we could change the outcome- which is obviously not the case. Infertility is not a "struggle," it is not a "fight," it is a medical problem that unfortunately afflicts many of us. Well-meaning friends and family may say "it will happen when you least expect it," or, "as soon as you stop trying you'll get pregnant." Well, quite honestly that is not true. Infertility is not something that can be changed by willpower, it is a medical condition that needs to be treated. Sometimes the cause of infertility can be pinpointed- I, for example, have one fallopian tube that is closed. But often there is no definitive reason. The conception of a child requires the combination of so many things to be perfectly in sync- it is no wonder so many couples cannot conceive! Hormones, endometrial health, ovarian health, egg count and age, and semen- all of this has to be functioning properly at the same time to allow a couple to become pregnant when they want. I will tell you our story. Thankfully, it has a happy ending. I met my husband, David, when I was 25 and got married at 27. At the time I was an anesthesiology resident at Georgetown University. We did not try for children right away. Working 80 hours a week and having a newborn did not feel feasible or enjoyable to me. And what little time off we did have we enjoyed going out and experiencing DC or traveling as much as we could afford. Fast forward a few years, I am now 30 and we have decided we want to start our family. Being a physician I knew it could take some time. I was not stressed the first month, or two, but after 6, 7, 8 months… I was both frustrated and concerned. Time seems to slip by when you are counting it in 4 week "cycles" tracking your period and peeing on a stick most mornings. Any couple who has actively tried to get pregnant knows the roller coaster: each month waiting to get the signal you're fertile, trying to conceive, hoping it worked, and then: either it does or it doesn't. And if it doesn't you are deflated but you know that next month- that could be it, that could be the month that it finally works! So you start all over again. Up and down, up and down. Please know, you are not alone on this roller coaster. Hopefully you have a supportive partner with you on the ride. But also, there are millions of women out there doing the same thing. If you are open about your experience you will likely find other women close to you that are on the ride with you. I will spare you all the details but we saw Elizabeth Irby, Women4Women CRNP, and did all the testing for myself and my husband. I do have a closed tube, but you should be able to get pregnant with just one tube so it is still partially unexplained. We tried fertility medication for a few months before deciding to move on to an infertility clinic. After conversation with our fertility specialist, Dr. Long, we opted to go forward with IVF using the invocelle. The invocelle is an awesome little device that allows you to incubate your embryos. After the eggs are fertilized, they are placed in a culture medium in the device and then inserted in the vagina where you incubate them for 5 days. Our first round we were so hopeful, we fertilized 3 good looking eggs. We went back after 5 days, and none of them had developed into usable embryos. I was not prepared for the level of heartbreak I felt at that moment. It was just a bunch of cells, right? But all of a sudden those 3 potential babies were gone in an instant from a glimpse at a microscope. And that was hard. My friends and family stepped up in a big way. I got flowers and well wishes and it bolstered us to try again. The second round of IVF worked. There is still a spot on my butt that is tender from all the progesterone injections, but I wouldn’t trade that for the world. Because our daughter, Rose, is now 4 months old and the most awesome part of our lives. She has a big gummy grin and chuckles like an old man and will completely melt your heart. Thankfully, I have had family and friends who were invested in this process with us. David and I made a conscious decision from the start to be open with those around us about what we were going through. You will be surprised when you start telling people what you are dealing with how many have their own story to contribute. We have made friendships built on the shared experience of infertility. I am glad we chose not to go through it alone. If you have not felt comfortable sharing with your friends and family, ask yourself why? Women have trouble recognizing that this is a disease inflicted upon them, not a failure. I have had the thought "if only I hadn't put off trying to get pregnant until after residency maybe we wouldn't have had to do IVF." But, maybe we would have? I will never know and guess what- it doesn't matter. There is no use thinking the "what ifs," or blaming yourself. I have never once blamed myself for having asthma, and I refuse to blame myself for having infertility. It is not your fault, it is not your body's fault. And that is why I believe Infertility Awareness Week is so important. I hope these stories empower women to be more open with their friends and families. You will be surprised- they want to be there for you, let them.